Nipah Virus – Comprehensive Detailed Article
Introduction

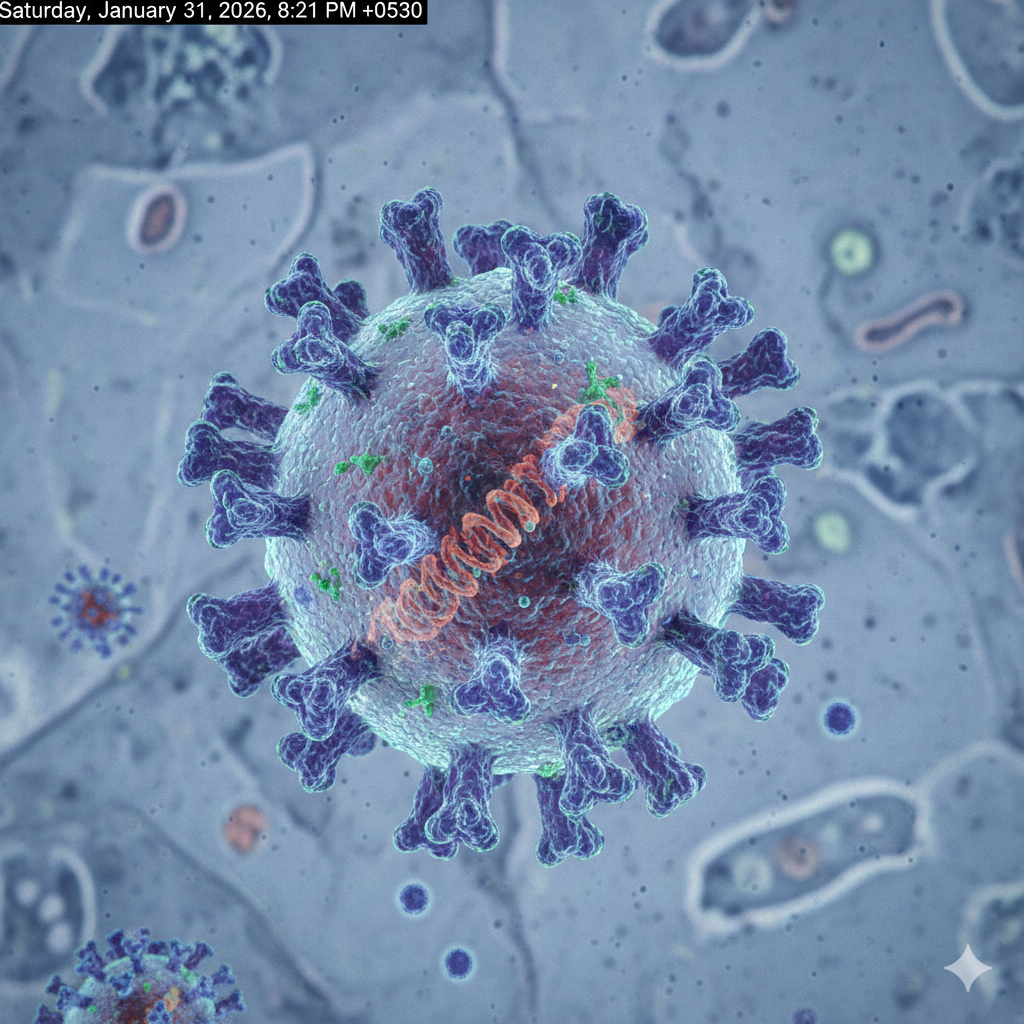
Nipah virus (NiV) is a highly lethal and emerging zoonotic virus that poses a serious threat to both human and animal health. It belongs to the Paramyxoviridae family and the Henipavirus genus. Infection with Nipah virus can cause severe respiratory illness, acute encephalitis (inflammation of the brain), and in many cases, death. Due to its high fatality rate and potential for human-to-human transmission, Nipah virus has been identified by global health authorities as a priority pathogen with epidemic potential.
This article provides a comprehensive and detailed overview of the Nipah virus, including its history, biological characteristics, transmission routes, symptoms, diagnosis, treatment, prevention strategies, public health impact, and future challenges.
History of Nipah Virus
Nipah virus was first identified during a major outbreak in 1998–1999 in Malaysia. The outbreak primarily affected pig farmers, where pigs acted as intermediate hosts transmitting the virus from fruit bats to humans. The virus was named after Sungai Nipah, a village in Malaysia where the first human cases were detected.
Following the Malaysian outbreak, additional outbreaks have been reported in Bangladesh, India (notably in West Bengal and Kerala), and Singapore. Unlike the Malaysian outbreak, later outbreaks—especially in Bangladesh and India—showed clear evidence of human-to-human transmission, increasing global concern about the virus.
Virological Characteristics
Nipah virus is a negative-sense, single-stranded RNA virus. It has a strong ability to replicate rapidly within host cells and evade immune responses.
Key Biological Features
- RNA virus with high mutation potential
- Zoonotic in nature (transmitted from animals to humans)
- High case fatality rate (approximately 40%–75%)
- Strong neurotropism (affects the brain)
- Capable of human-to-human transmission
Natural Reservoirs
The natural reservoirs of Nipah virus are fruit bats of the genus Pteropus, commonly known as flying foxes. These bats carry the virus without showing symptoms and shed it through saliva, urine, feces, and partially eaten fruits.
Transmission to humans can occur either directly from bats or indirectly through intermediate animal hosts such as pigs.
Modes of Transmission
Nipah virus can spread through several routes:
1. Animal-to-Human Transmission
- Direct contact with infected pigs or other animals
- Exposure to animal secretions such as blood, urine, or saliva
2. Bat-to-Human Transmission
- Consumption of fruits contaminated by bat saliva or urine
- Drinking raw date palm sap contaminated by bats
3. Human-to-Human Transmission
- Close contact with infected individuals
- Exposure to bodily fluids (respiratory droplets, saliva, urine)
- Inadequate infection control practices in healthcare settings
Incubation Period
The incubation period of Nipah virus typically ranges from 4 to 14 days, but in some cases, it may extend up to 45 days.
Clinical Manifestations
Early Symptoms
- Fever
- Headache
- Muscle pain
- Vomiting
- Fatigue
Severe Symptoms
- Acute respiratory distress
- Encephalitis (brain inflammation)
- Dizziness and altered consciousness
- Seizures
- Coma
In severe cases, rapid neurological deterioration may occur within 24–48 hours.
Diagnosis
Laboratory confirmation of Nipah virus infection requires specialized facilities due to the virus’s high risk.
Diagnostic Methods
- Reverse Transcriptase Polymerase Chain Reaction (RT-PCR)
- Enzyme-Linked Immunosorbent Assay (ELISA)
- Virus isolation (restricted to BSL-4 laboratories)
Samples may include blood, urine, throat swabs, and cerebrospinal fluid (CSF).
Treatment
Currently, there is no specific antiviral treatment or licensed vaccine for Nipah virus infection.
Supportive Care
- Intensive care unit (ICU) management
- Mechanical ventilation for respiratory failure
- Management of seizures and brain swelling
- Fluid and electrolyte balance
Experimental therapies and monoclonal antibodies are under investigation but are not yet widely available.
Prevention and Control
Prevention remains the most effective strategy against Nipah virus.
Key Preventive Measures
- Avoid consumption of raw date palm sap
- Wash and peel fruits thoroughly before eating
- Prevent bat access to food and water sources
- Use personal protective equipment (PPE) when caring for patients
- Implement strict infection prevention and control measures in hospitals
Public Health Impact
Nipah virus outbreaks place immense pressure on public health systems. High mortality rates, fear of contagion, and lack of definitive treatment often lead to social disruption, economic losses, and strain on healthcare resources.
Due to its pandemic potential, Nipah virus is included in the World Health Organization (WHO) Blueprint Priority Diseases list.
Research and Future Challenges
Significant research efforts are ongoing to develop effective vaccines, antiviral drugs, and rapid diagnostic tools. Strengthening disease surveillance, improving laboratory capacity, and enhancing public awareness are crucial to preventing future outbreaks.
Climate change, deforestation, and increased human–animal interaction are expected to increase the risk of Nipah virus emergence in new regions.
Conclusion
Nipah virus is one of the most dangerous emerging infectious diseases known today. Its high fatality rate, lack of specific treatment, and potential for human-to-human transmission make it a serious global health concern. Until effective vaccines and treatments are developed, prevention, early detection, and strong public health measures remain the cornerstone of control.
This article serves as a comprehensive guide to understanding Nipah virus and highlights the urgent need for continued research and preparedness.
Global Perspectives: How Different Countries Address Nipah Virus
Different countries respond to the Nipah virus based on their exposure risk, healthcare capacity, surveillance systems, and past outbreak experiences. Below is a detailed overview of how various regions view, monitor, and manage the Nipah virus.
Bangladesh
Bangladesh experiences nearly annual Nipah outbreaks, making it one of the most affected countries.
Key Characteristics:
- Primary transmission via raw date palm sap contaminated by fruit bats
- Frequent human-to-human transmission
- High fatality rate (often above 70%)
Response Strategy:
- Nationwide surveillance during date palm harvesting season
- Public education campaigns discouraging raw sap consumption
- Rapid isolation and contact tracing
- Collaboration with WHO and CDC for outbreak control
Bangladesh treats Nipah virus as a recurring national public health emergency.
India
India has reported multiple outbreaks, mainly in West Bengal and Kerala.
Key Characteristics:
- Strong evidence of human-to-human transmission
- High public awareness due to media coverage
Response Strategy:
- Immediate lockdowns and containment zones during outbreaks
- Advanced contact tracing and quarantine measures
- High-level biosafety laboratories (BSL-4) for diagnostics
- National task forces activated during outbreaks
India considers Nipah virus a high-priority emerging infectious disease.
Malaysia
Malaysia was the site of the first recorded Nipah outbreak.
Key Characteristics:
- Transmission mainly from pigs to humans
- Large economic losses due to pig culling
Response Strategy:
- Strict animal health surveillance
- Biosecurity regulations for livestock farming
- Long-term monitoring of pig farms
Malaysia now focuses on animal-to-human transmission prevention.
Singapore
Singapore recorded cases linked to imported pigs during the Malaysian outbreak.
Response Strategy:
- Immediate ban on pig imports from affected regions
- Strict food safety and border controls
- Hospital preparedness protocols
Singapore views Nipah virus primarily as a biosecurity and import-related risk.
Australia
Australia has Henipaviruses closely related to Nipah (e.g., Hendra virus).
Response Strategy:
- Advanced zoonotic disease surveillance
- Strong wildlife monitoring programs
- High-level laboratory research
Australia treats Nipah virus as a potential future spillover threat.
United States
The U.S. has not experienced Nipah outbreaks but classifies it as a high-risk pathogen.
Response Strategy:
- Classified as a Biosafety Level-4 (BSL-4) pathogen
- Intensive research through CDC and NIH
- Vaccine and monoclonal antibody development
The U.S. views Nipah virus as a global health security threat.
European Union
Europe has no recorded outbreaks but considers Nipah virus a cross-border health risk.
Response Strategy:
- Travel surveillance and risk assessments
- Research funding for emerging pathogens
- Pandemic preparedness planning
World Health Organization (WHO)
The WHO classifies Nipah virus under Blueprint Priority Diseases.
WHO Focus Areas:
- Global surveillance and early warning systems
- Supporting vaccine and therapeutic research
- Assisting countries with outbreak preparedness
Conclusion
Globally, Nipah virus is viewed not as a local disease but as a potential pandemic threat. Countries with previous outbreaks focus on containment and prevention, while others invest in preparedness, research, and surveillance. International cooperation remains essential to prevent future large-scale outbreaks.
Home-Based Preventive Measures (What Should Be Done at Household Level)
Preventing Nipah virus infection at the household level is extremely important, especially in regions at risk or during outbreaks. Since there is no specific cure or vaccine, home-based preventive practices play a critical role in reducing transmission.
1. Food Safety at Home
- Always wash fruits thoroughly with clean water before eating
- Peel fruits whenever possible, especially those that may have been exposed to bats
- Do not consume fruits that are partially eaten or damaged
- Avoid consuming raw or unboiled date palm sap
Food hygiene is one of the most effective household-level preventive strategies.
2. Avoid Contact with Bats and Wild Animals
- Do not touch bats, even if they appear sick or dead
- Keep children away from bats and other wild animals
- Prevent bats from entering homes by covering open roofs and windows
3. Maintain Personal Hygiene
- Wash hands frequently with soap and water
- Use alcohol-based hand sanitizers when soap is unavailable
- Avoid touching the face (eyes, nose, mouth) with unwashed hands
4. Care of Sick Family Members
- Isolate family members showing fever, breathing difficulty, or neurological symptoms
- Avoid direct contact with bodily fluids (saliva, urine, vomit)
- Caregivers should use masks and gloves if possible
- Seek medical attention immediately if symptoms worsen
5. Respiratory Hygiene
- Cover mouth and nose when coughing or sneezing
- Dispose of tissues safely
- Wear masks when caring for sick individuals
6. Clean Household Environment
- Clean surfaces regularly using disinfectants
- Properly dispose of waste
- Ensure good ventilation inside the house
7. Community Awareness at Home
- Educate family members about Nipah virus symptoms and transmission
- Follow instructions issued by health authorities
- Avoid unnecessary travel during outbreak periods
8. When to Seek Medical Help
Immediately seek medical care if any family member develops:
- High fever
- Severe headache
- Difficulty breathing
- Confusion or seizures
Early medical intervention can save lives.
Conclusion
Globally, Nipah virus is viewed not as a local disease but as a potential pandemic threat. Countries with previous outbreaks focus on containment and prevention, while others invest in preparedness, research, and surveillance. International cooperation remains essential to prevent future large-scale outbreaks.
🌐 External Resources – DoFollow Links (Copy‑Paste)
🔹 World Health Organization (WHO) – Nipah Virus Fact Sheet
https://www.who.int/news-room/fact-sheets/detail/nipah-virus
🔹 Centers for Disease Control and Prevention (CDC) – About Nipah Virus
https://www.cdc.gov/nipah-virus/about/index.html
🔹 World Organisation for Animal Health (WOAH) – Nipah Virus Disease
https://www.woah.org/en/disease/nipah-virus/
🔹 European Centre for Disease Prevention and Control (ECDC) – Nipah Virus Info
https://www.ecdc.europa.eu/en/news-events/nipah-virus-disease-cases-reported-west-bengal-india-very-low-risk-europeans
📌 Suggested Placement in Article
🔹 External Resources (DoFollow – Trusted Health Organizations)
For the most reliable and up‑to‑date information on Nipah virus, visit these authoritative sources:
- 🌍 World Health Organization (WHO) – Nipah Virus Fact Sheet: https://www.who.int/news-room/fact-sheets/detail/nipah-virus
- 🦠 Centers for Disease Control and Prevention (CDC) – About Nipah Virus: https://www.cdc.gov/nipah-virus/about/index.html
- 🐾 World Organisation for Animal Health (WOAH) – Nipah Virus Disease: https://www.woah.org/en/disease/nipah-virus/
- 🇪🇺 European Centre for Disease Prevention and Control (ECDC) – Nipah Virus Risk Updates: https://www.ecdc.europa.eu/en/news-events/nipah-virus-disease-cases-reported-west-bengal-india-very-low-risk-europeans
Explore More on Health and Wellness
At Health Guide Me, we offer a variety of detailed articles to support your health journey. Below are some recommended reads:
- Health Guide Me – Trusted Health Information
The homepage provides access to comprehensive health guides, expert tips, and evidence-based articles covering a wide range of health topics, from nutrition to preventive care. - Probiotics Benefits for Gut Health
This article explains the importance of probiotics for maintaining digestive health, boosting immunity, and promoting overall well-being. It highlights how gut health is connected to disease prevention and long-term health. - Protein Supplements and Protein-Rich Foods
Learn about different protein sources, their benefits for muscle growth and overall health, and practical tips for incorporating protein supplements and high-protein foods into your diet.